Nowadays, many places we visit have some form of digital or 3D map showing us a blueprint of the place; airports, shopping malls, and even city centers. Yet in hospital settings, it’s still pretty uncommon. Through the introduction of accessible mapping and tracking which can be accessed via kiosks or mobile phones, patients and practitioners will have a clearer view of where they need to be.
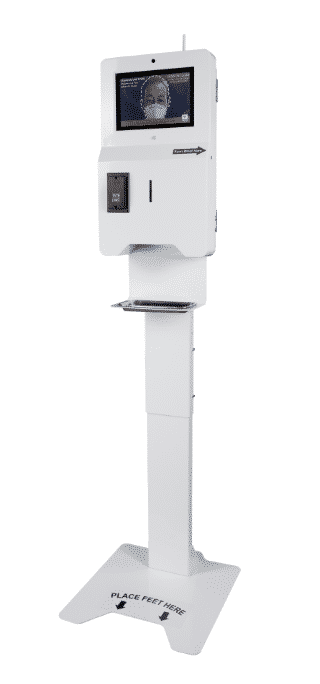
Although digital check-in in hospitals has increased over the last few years, this, unfortunately, is usually the limit of its use. Now, however, forward-thinking hospitals have the chance to create a much more user-friendly, fluid interface where check-in kiosks are integrated with digital mapping technology and signage making hospital wayfinding in the biggest facilities much easier.
How exactly does this work?
Upon check-in, interactive maps on the screen will allow the user to see exactly where they need to be in the hospital. Then, for those who have smartphones, the hospital map can be downloaded in seconds so they can be guided the entire way.
Maps can be downloaded in multiple ways, but the most practical is either by scanning a QR code or with a text link sent to the user’s mobile. This can then open up a webpage with the map and ‘blue dot’ tracking, or prompt the user to download an app for a more optimized experience.
Of course, there are some accessibility concerns with hospital mobile wayfinding, especially when considering the older population. They may not have access to a smartphone or know how to use digital signage tech effectively enough for it to work. However, in these scenarios, digital kiosks placed at intersections of the hospital could act as a guide, as well as overhead signage, which is a dramatic improvement on traditional methods of wayfinding.
The Bottom Line
Digital signage presents a unique opportunity to overcome one of the biggest issues people face when visiting large hospitals. It allows for a smoother visit and fewer missed appointments, saving time and money for both patient and medical professionals.
The introduction of intuitive and accessible digital signage will not just give visitors and patience a better experience, but staff will be able to navigate easier, even when they’re new to the hospital, and wait times could even be decreased due to more streamlined operations.
In short, hospital mapping and wayfinding with digital signage and touch screen kiosks is an ideal solution for improving patient experience and increasing the efficiency of your hospital. It provides a technological boost that can help set a hospital apart from others.